On the surface it seems simple. If you’re sick, you find a doctor, get treated and eventually get to feeling better. Unfortunately, the system has become unnecessarily complicated, and poor patient experience has financial consequences for employers.
Think about your last doctor’s appointment:
This story isn’t unique. Nearly one-third of respondents in a recent national survey reported avoiding going to the doctor, even those diagnosed with major health problems or were experiencing worrisome symptoms. Whether due to lack of convenient access, previous experiences or misunderstanding of cost, avoiding or delaying care can quickly turn a controllable condition into an emergency.
Take, for example, the symptoms of diabetes: fatigue, extreme thirst, a cough that won’t seem to go away. Disregarding these symptoms and avoiding care can delay diagnosis, one that can be managed through treatment and lifestyle changes.
Left untreated or under-treated, diabetes can lead to nerve and kidney damage, stroke and even death. Employees can also often delay care for conditions that can eventually land them in the emergency room. Poor management of chronic conditions and catastrophic emergency events increase the chance for significant claims and poor health outcomes, when earlier intervention would have been more cost-effective and better for the patient.
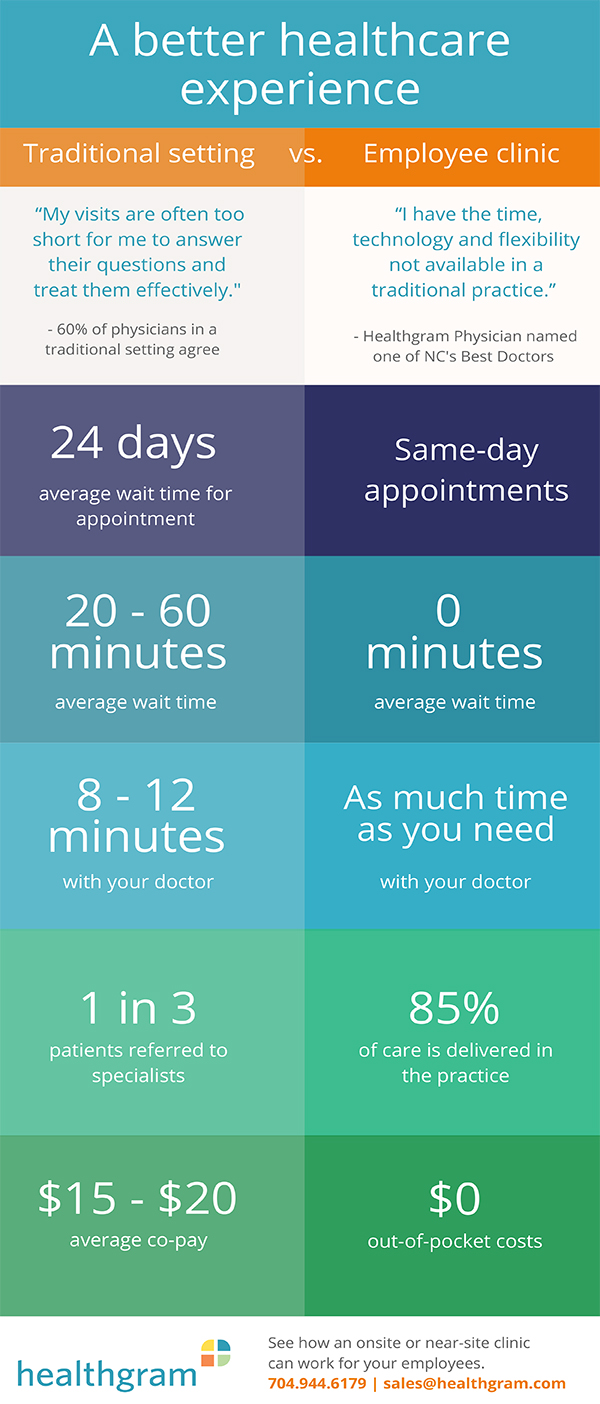
In these arrangements, employers give employees access to high-quality, physician-led care in near-site, onsite or shared multi-employer clinics independent of traditional employer-sponsored insurance. The idea is to provide convenient, more comprehensive and personal care that encourages earlier intervention. Over time, employees enjoy better health and employers reduce costs.
Sources:
American Journal of Managed Care, Opportunity Costs of Ambulatory Medical Care in the United States
Vitals Wait Time Report
Kaiser Family Foundation